This activity is provided by Med Learning Group.
This activity is supported by an independent medical education grant from Regeneron Pharmaceuticals, Inc.
Copyright © 2024 Med Learning Group. Built by Divigner. All Rights Reserved.
Diagnosis and staging
Non-Hodgkin’s Lymphoma Diagnosis and Staging
For all types of non-Hodgkin’s lymphoma diagnosis, an essential workup would include several blood tests and exams including the following:2,3
- History: B symptoms
- Physical exam: with attention to node-bearing areas, and to the size of the liver and spleen
- Performance status
- Serology: Hepatitis B, C, HIV
- Blood tests: CBC with differential, LDH, Comprehensive metabolic panel, Pregnancy panel, beta-2-microglobulin
- Imaging: PET/CT scan (including neck) with contrast, PET/CT scan and/or chest/abdominal/pelvic CT with contract of diagnostic quality, abdominal ultrasound, endoscopy/colonoscopy
- Bone marrow: Bone marrow biopsy + aspirate, histology, cytology, immunophenotyping (IHC panel or cell surface marker analysis by flow cytometry with peripheral blood and/or biopsy specimen)
- Toxicity: creatinine clearance, uric acid, ECG/MUGA scan, cardiac ultrasound (before anthracyclines), pulmonary function (ASCT)
- Lumbar puncture
- Molecular analysis: Karyotype or FISH
For all B-cell lymphomas, diagnosis is confirmed via excisional or incisional biopsy, and a fine needle aspiration (FNA) biopsy on its own is not considered suitable for initial non-Hodgkin’s lymphoma diagnosis. A combination of core needle biopsy (preferably multiple biopsies) and FNA biopsies in conjunction with other techniques such as immunohistochemistry (IHC), flow cytometry, and molecular analysis for the detection of immunoglobulin gene rearrangements, karyotype, or FISH for major translocations) may be sufficient for a non-Hodgkin’s lymphoma diagnosis. Additionally, a hematopathology review of all slides with at least one paraffin block representative of the tumor is required.2 Additional diagnostic blood tests and exams for non-Hodgkin’s lymphoma, focusing on each unique type, may be required and information about these can be found in the Resources section.
Non-Hodgkin’s Lymphoma Staging
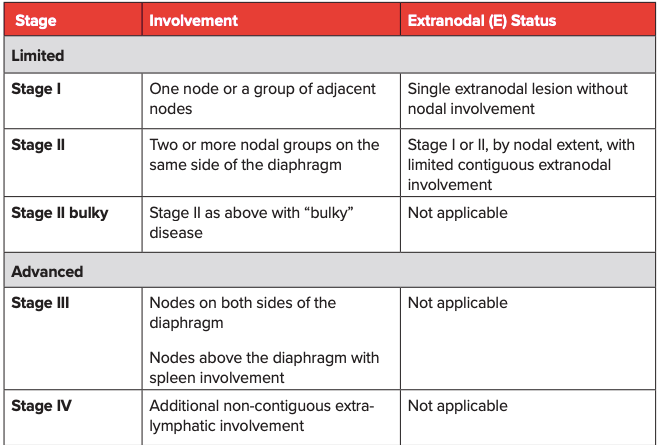
Non-Hodgkin’s lymphoma staging is a way to determine where the cancer is, and how much it has spread to other sites. A thorough staging will help determine the best course of treatment.3 Non-Hodgkin’s lymphoma staging is typically carried out according to the Ann Arbor classification system (Table 1), with a mention of bulky disease when that is applicable. For follicular lymphoma (FL), an FL International Prognostic Index or FLIPI that considers nodal sites (>4 lymph nodes), age (>60 years), serum marker (elevated LDH), stage of disease (advanced Ann Arbor classification stage III-IV), and hemoglobin to categorize patients into low risk (0-1 risk factor), intermediate risk (2 risk factors), and high risk (3-5 risk factors) has been established. For patients requiring treatment, a revised FLIPI2 score that incorporates beta-2-microglobulin, the diameter of the largest lymph node, bone marrow involvement, and hemoglobin levels is available.3
Table 1: Lugano modification of the Ann Arbor Staging System (for primary nodal lymphomas)1
References
- Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging and response assessment of Hodgkin and non-Hodgkin’s lymphoma: The Lugano classification. J Clin Oncol. 2014;32:3059-3067. https://doi.org/10.1200/JCO.2013.54.8800
- National Comprehensive Cancer Network®. NCCN Clinical Practice Guidelines in Oncology. B-Cell Lymphomas. Version 5.2022. July 12, 2022. https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf
- Dreyling M, Ghielmini M, Rule S, et al. Newly diagnosed and relapsed follicular lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32:298-308. https://doi.org/10.1016/j.annonc.2020.11.008