Defining Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma (NHL) is a heterogeneous group of cancers that originate in the lymphoid system and that spread in a disorderly manner, often to extranodal sites.1,2 NHL has diverse genotypes, immunologic phenotypes, molecular biology, morphology, and clinical characteristics.3
There are several novel biomarkers that are being investigated at the genetic, epigenetic, and protein levels, and in the tumor microenvironment, that can potentially provide insights into the processes underlying lymphomagenesis and aid in diagnosis, classification, outcome stratification, and personalizing patient treatment.4
Subtypes
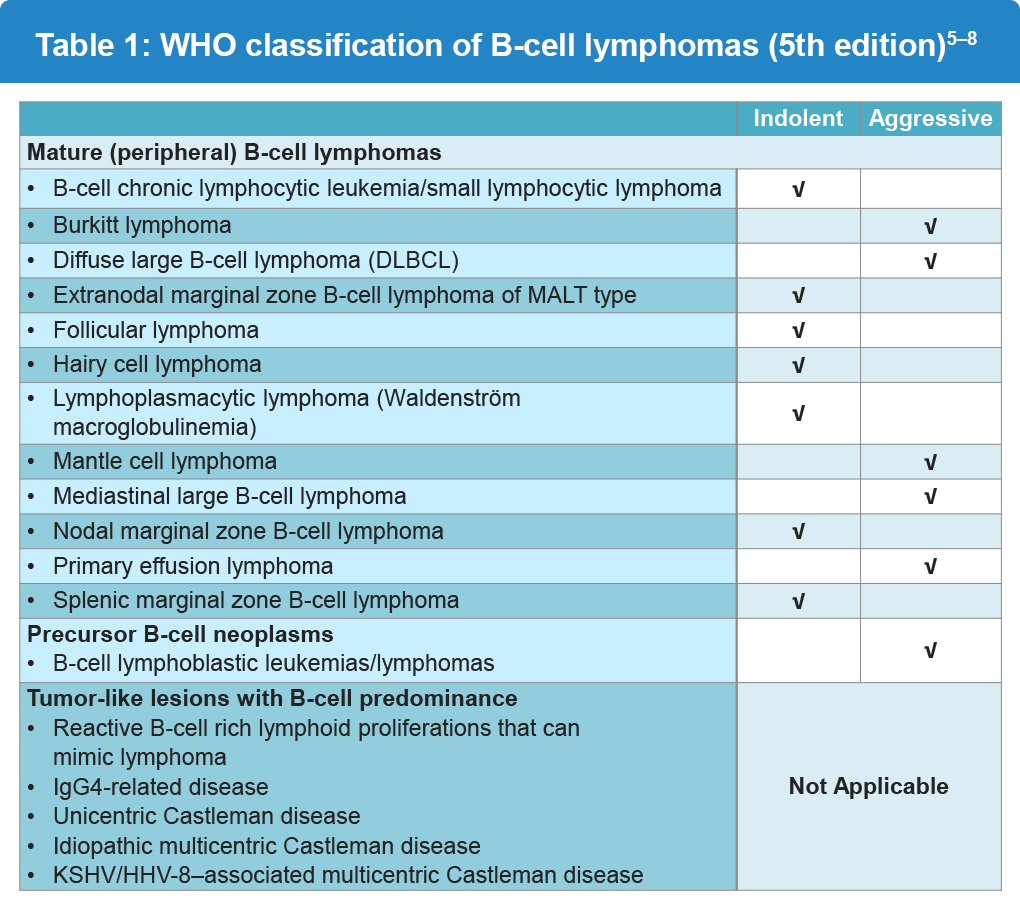
There are over 60 major subtypes of NHL, with follicular lymphoma (FL) being the most common indolent type of NHL and diffuse large B-cell lymphoma (DLBCL) being the most common aggressive type of NHL.5 There is no ‘gold standard’ for classifying the various types of NHL; however, cancers are generally grouped by using a combination of morphology, immunophenotype, and clinical and genetic features (Table 1).1 The focus of this website is on B-cell neoplasms.
Epidemiology
NHL is the 8th most common type of cancer and the eighth leading cause of cancer-related death in the US. In 2025, it is estimated that approximately 80,350 new cases of NHL will be diagnosed and about 19,390 people will die of NHL in the US.8,9
The 5-year survival rate based on data from 2014-2020 was 74.2%. The incidence of NHL has declined by about 0.6% per year since 2013. And, from 2014 to 2023, the death rate decreased by 2% per year.10
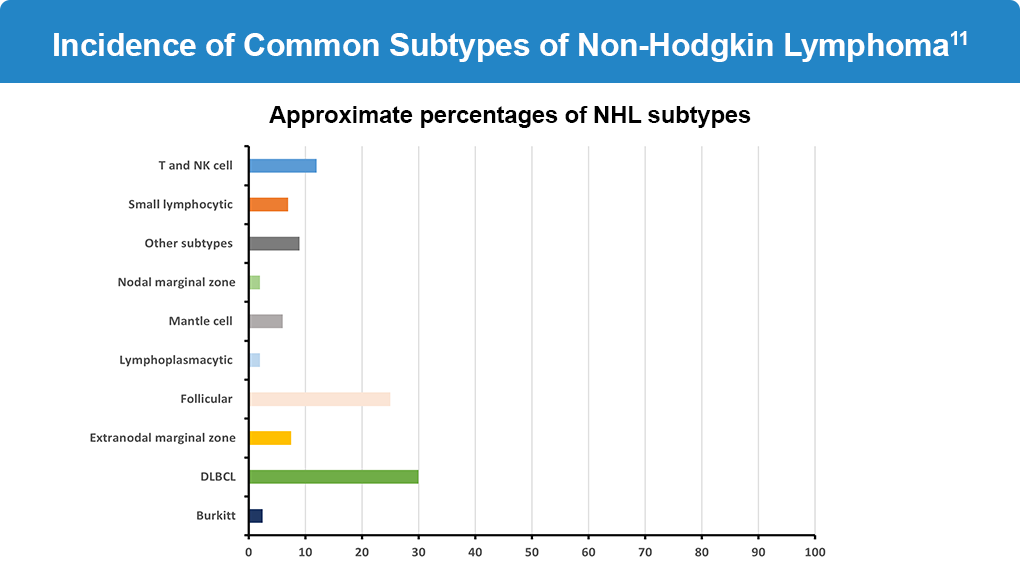
The incidence of NHL subtypes varies by geographical region.11 Diffuse large B-cell lymphoma (DLBCL) is the most common aggressive form of NHL in Western countries (30%) followed by mantle cell lymphoma (6%) and Burkitt’s lymphoma (2%), and follicular lymphoma (FL) is the most common indolent form of NHL (25%), followed by marginal zone lymphoma (7.5%), chronic lymphocytic leukemia/small-cell lymphocytic leukemia (CLL/SLL; 6%), and lymphoplasmacytic lymphoma (LPL; 1%) (Figure 1). Newly available therapies such as CD19-targeted chimeric antigen receptor T-cell therapies, bispecific anti-CD20 antibodies and antibody-drug conjugates have contributed to these improved outcomes.10,12
Risk Factors
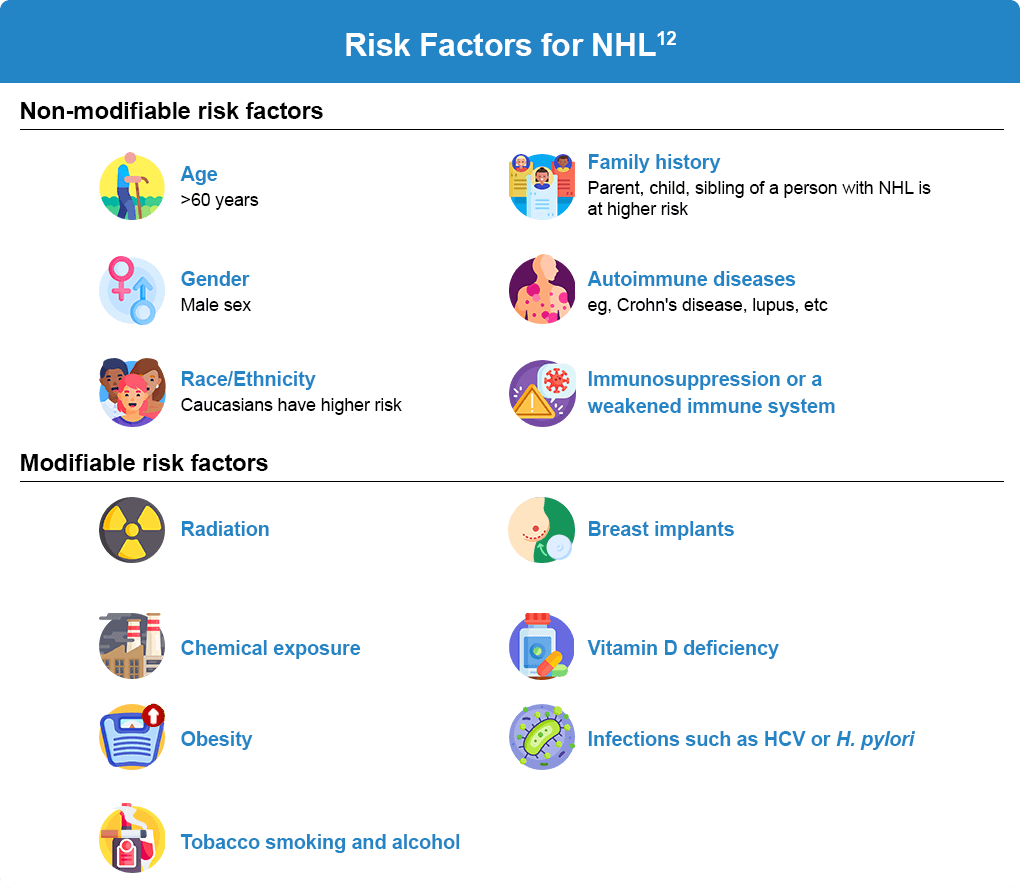
The International Lymphoma Epidemiology Consortium (InterLymph) was established in 2001 to address the heterogeneity of NHL and determine specific mechanisms and risk factors for various subtypes.10 Although not all people with risk factors develop NHL, preventive measures aimed at reducing the modifiable risk factors could significantly reduce the risk of developing NHL.13
References:
- Singh R, Shaik S, Negi BS, et al. Non-Hodgkin’s lymphoma: A review. J Family Med Prim Care. 2020;9:1834-1840. doi:10.4103/jfmpc.jfmpc_1037_19
- Nogai H, Dörken B, Lenz G. Pathogenesis of non-Hodgkin’s lymphoma. J Clin Oncol. 2011;29:1803-1811. doi:10.1200/JCO.2010.33.3252
- Pavlovsky M, Cubero D, Agreda-Vásquez GP, et al. Clinical outcomes of patients with B-cell non-Hodgkin lymphoma in real-world settings: Findings from the Hemato-Oncology Latin America Observational registry study. JCO Glob Oncol. 2022;8:e2100265. doi:10.1200/GO.21.00265
- Sun R, Medeiros LJ, Young KH. Diagnostic and predictive markers for lymphoma diagnosis and treatment in the era of precision medicine. Mod Pathol. 2016;29:1118-1142. doi:10.1038/modpathol.2016.92
- Blood Cancer United. Non-Hodgkin lymphoma (NHL) diagnosis. (https://bloodcancerunited.org/blood-cancer/lymphoma/non-hodgkin-lymphoma/diagnosis).
- Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization Classification of hematolymphoid tumors: Lymphoid neoplasms. Leukemia. 2022;36:1720-1748. doi:10.1038/s41375-022-01620-2
- Di Rocco A, Petrucci L, Assanto GM, Martelli M, Pulsoni A. Extranodal marginal zone lymphoma: Pathogenesis, diagnosis and treatment. Cancers (Basel). 2022;14:1742. doi:10.3390/cancers14071742
- Teklie Y, Bell S, Idogun P, Venigalla M. A rare case of a patient with hairy cell leukemia developing blastoid marginal zone B-cell lymphoma. Cureus. 2021;13:e16239. doi:10.7759/cureus.16239
- Luo J, Craver A, Bahl K, et al. Etiology of non-Hodgkin lymphoma: A review from epidemiologic studies. J Nat Cancer Center. 2022;2:226-234. doi:10.1016/j.jncc.2022.08.003
- National Cancer Institute. SEER Cancer Stat Facts: Non-Hodgkin Lymphoma. (https://seer.cancer.gov/statfacts/html/nhl.html).
- Armitage JO, Weisenburger DD. New approach to classifying non-Hodgkin’s lymphomas: Clinical features of the major histologic subtypes. Non-Hodgkin’s Lymphoma Classification Project. J Clin Oncol. 1998;16:2780-2795. doi:10.1200/JCO.1998.16.8.2780
- National Comprehensive Cancer Network®. NCCN Clinical Practice Guidelines in Oncology. B-Cell Lymphomas. Version 3.2025. https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf
- Thandra KC, Barsouk A, Saginala K, Padala SA, Barsouk A, Rawla P. Epidemiology of non-Hodgkin’s lymphoma. Med Sci (Basel). 2021;9:5. doi:10.3390/medsci9010005
ALL URLs accessed October 27, 2025