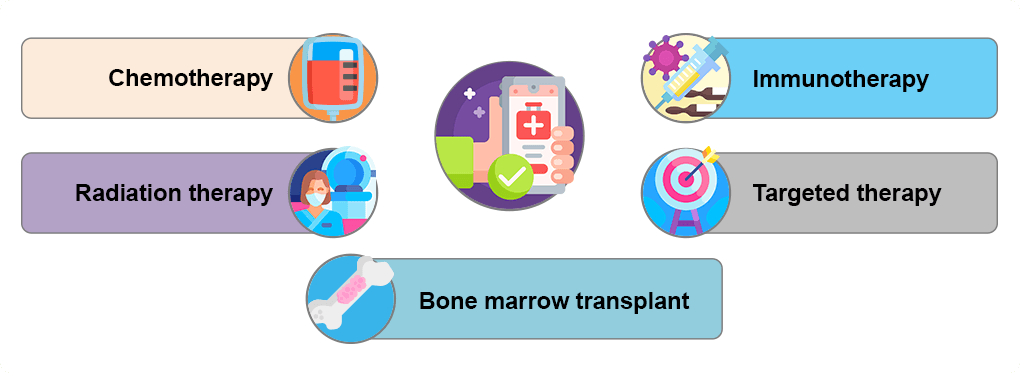
Treatment and Management of NHL
Current treatments for NHL
A wide range of treatments is currently available to treat non-Hodgkin lymphoma (NHL). Treatment choices depend on the specifics of your lymphoma, including the type and location and whether it is aggressive or indolent. Lymphomas that are indolent may not need immediate treatment, but rather monitoring to see if they are advancing.1 Treatments are broadly divided into the following five categories, with recommended options based on overall health and individual preferences:
Chemotherapy
Chemotherapy is one of the main treatments for NHL and may be given alone or in combination with other treatments depending on the NHL type and stage. Generally given orally or intravenously (IV), it destroys fast-growing cancer cells.4 Chemotherapy drugs are typically given in cycles, with periods of treatment usually lasting several weeks followed by periods of recovery where no treatment is given. The most common regimen of chemotherapy is called CHOP and consists of four medications: cyclophosphamide, doxorubicin, prednisone, and vincristine. Often, monoclonal antibodies called rituximab (R-CHOP) or obinutuzumab (O-CHOP) are added to this regimen. Other chemotherapy regimens include combinations of drugs, such as bendamustine and rituximab, fludarabine, and R-CVP (rituximab, cyclophosphamide, vincristine sulfate, and prednisone). More recently, Pola-R-CHP (polatuzumab vedotin, rituximab, cyclophosphamide, doxorubicin, and prednisone) has become an option for large B-cell lymphomas.3 Chemotherapy may also be used to prepare your body for a bone marrow or stem cell transplant.1,2
Radiation Therapy
Utilizes high energy beams, such as X-rays or other types of radiation to destroy cancer cells. Radiation can be used alone to target one or two targeted sites that contain lymphoma and can be used after chemotherapy to destroy any remaining lymphoma cells.2 Treatments are often given 5 days per week over several weeks.5
Immunotherapy
Uses a patient’s own immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s immune defenses. Chimeric antigen receptor (CAR) T-cell therapy and immune checkpoint inhibitors are two immunotherapies available for treatment of NHL.1,2
CAR T-cell therapy includes the use of modified T cells to target cancer. In CAR T therapy some of the patient’s own T cells are removed and modified to contain specific proteins called receptors. The receptors allow these modified T cells to recognize cancer cells having the target protein that these receptors bind to. These modified T cells are expanded in a lab and then returned to the patient’s body. Currently available FDA-approved CAR T therapies include axicabtagene ciloleucel, tisagenlecleucel, brexucabtagene autoleucel, and lisocabtagene maraleucel.1-3
Immune checkpoint inhibitors block immune checkpoints that cancer cells use to evade detection, preventing the immune system from attacking healthy cells and allowing it to target cancer. Pembrolizumab is an example of such an inhibitor.1
Targeted Drug Therapy
Targets specific cancer cells and blocks the abnormalities causing cancer.1 Different types of targeted therapies are listed below:
Monoclonal antibodies are lab-produced proteins that mimic the immune system. These antibodies attach to a specific target on cancer cells to help destroy them and prevent them from spreading. They are administered by intravenous infusion. Examples of monoclonal antibodies include rituximab, obinutuzumab and ofatumumab which target a protein called CD20 and tafasitamab which targets CD19.1
Radiolabeled antibodies contain radioactive material that targets cancer cells; an example is ibritumomab tiuxetan.1
Antibody-drug conjugates attach to cancer cells and release a drug directly into the tumor cells. Examples of anti-body drug conjugates include brentuximab, loncastuximab tesirine-lpyl, and polatuzumab vedotin piiq.2,3
Bispecific antibodies (BsAbs) are designed to recognize two different targets expressed on a cell surface, called antigens. These medicines can be administered intravenously (IV) or subcutaneously (SC, which is underneath the skin). Once in the bloodstream, BsAbs travel throughout the body and attach themselves to the cell(s) that express their specific antigens.6
The key difference between standard antibodies and bsAbs is based on their mechanism of action. Natural antibodies (produced by the body’s immune system) and monoclonal antibodies used in therapy, interact with a single antigen in the cell that is being targeted. On the other hand, BsAbs target more than one antigen; they are less susceptible to drug resistance compared to standard monoclonal antibodies, especially in diseases that are caused by multiple factors, such as cancer. Examples of BsAbs include glofitamab, epcoritamab, mosunetuzumab, and odronextamab. 6,7
Further details on each of these therapies can be accessed in the Resources section.2,3
Bone Marrow Transplant/Stem Cell Transplantation
Involves using high doses of radiation and chemotherapy to suppress the patient’s bone marrow and immune system. Healthy bone marrow or stem cells is then infused into the patient’s blood to travel to the bone marrow to regenerate healthy immune system bone marrow. Depending on the source of the stem cells, the transplant may be considered autologous (patient’s own stem cells) or allogenic (donor stem cells).2,8
References:
- Mayo Clinic. Non-Hodgkin lymphoma. Diagnosis and Treatment. November 7, 2025. (https://www.mayoclinic.org/diseases-conditions/non-hodgkins-lymphoma/diagnosis-treatment/drc-20375685)
- American Cancer Society. Treating Non-Hodgkin Lymphoma. (https://www.cancer.net/cancer-types/lymphoma-non-hodgkin/types-treatment)
- PDQ Adult Treatment Editorial Board. Non-Hodgkin’s Lymphoma Treatment (PDQ®): Patient Version. In: PDQ Cancer Information Summaries. National Cancer Institute. August 22, 2024. (https://www.ncbi.nlm.nih.gov/books/NBK65899/).
- American Cancer Society. Non-Hodgkin Lymphoma Stages. Last Revised: February 15, 2024. (https://www.cancer.org/cancer/types/non-hodgkin-lymphoma/detection-diagnosis-staging/staging.html)
- American Cancer Society. Radiation Therapy for Non-Hodgkin Lymphoma. Last Revised: February 15, 2024. (https://www.cancer.org/cancer/types/non-hodgkin-lymphoma/treating/radiation-therapy.html)
- Lymphoma Research Foundation. Understanding Lymphoma and Chronic Lymphocytic Leukemia (CLL): Bispecific antibodies. Last updated May 2024. (https://lymphoma.org/wp-content/uploads/2024/10/Bispecific_Antibodies_Fact_Sheet_2024.pdf).
- National Comprehensive Cancer Network®. NCCN Clinical Practice Guidelines in Oncology. B-Cell Lymphomas. Version 3.2025. (https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf)
- Lymphoma Research Foundation. Understanding lymphoma and Chronic Lymphocytic Leukemia (CLL). Non-Hodgkin Lymphoma (Lymphoid Neoplasms). Last updated May 2024. (https://lymphoma.org/wp-content/uploads/2024/10/Non_Hodgkin_Lymphoma_Fact_Sheet_2024.pdf
ALL URLs accessed October 28, 2025